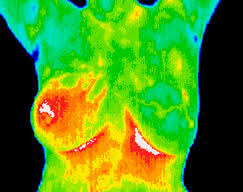
Machine learning and infrared thermal imaging in breast cancer detection
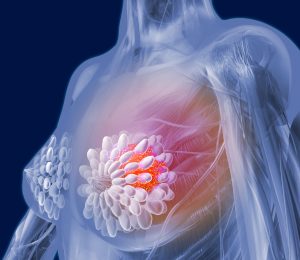
Cancer is the most important public health issue in the world and breast cancer is the most commonly cancer type detected in American women. Breast cancer is the second type more common cancers in the world and is more widespread among women.
Over the past 20 years, many applications have been found in the medical profession for early detection of breast cancer such as mammography which is often used for breast cancer diagnosis.
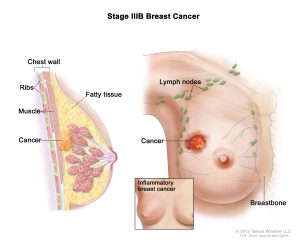
However, the potential side effects of using mammography and the rate of false positives discourages patients and physicians to use this method. Moreover, mammography has some limitations such as the difficulty of detecting tumors in young patients or cancers without masses, such as Paget’s carcinoma. Since the young breast is mainly composed of glandular tissue, which makes it denser, this high density of the breast interferes in the identification of masses and micro-calcifications by X-rays.
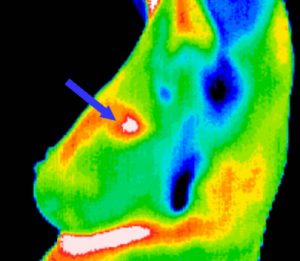
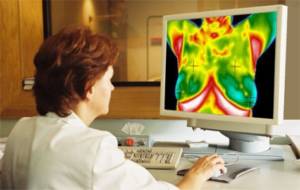
Infrared thermography (IRT) is another technique that has been used in combination with other screening techniques in the aid of breast cancer detection. This method is:
- A low-cost technique that does not involve harmful radiation to humans
- It does not involve invasive procedures
- It is based on the principle of measuring the infrared radiation emitted by an object or surface through an infrared camera to determine its temperature
- It may provide better results for breast cancer detection in young women, who usually have denser breasts, when compared to mammography
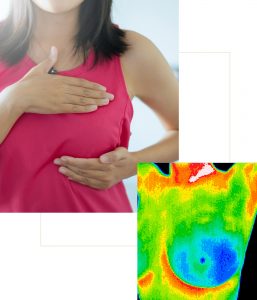
The approach proposed in this article: Gonçalves, C.B; Leles, A.C.Q.; Oliveira, L.E.; Guimaraes, G.; Cunha, J.R.; Fernandes, H. Machine Learning and Infrared Thermography for Breast Cancer Detection. Proceedings 2019, 27, 45 involves the acquisition of infrared images of healthy patients and patients with cancer followed by the extraction of features to describe these images.
Database
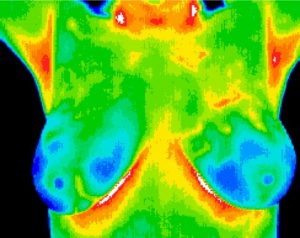
The database used contains data from 70 patients with or without breast tumor. These images were collected in a five-month period. The images were captured with a mid-wave infrared camera.
Images were acquired using the static protocol:
- Patient waited 15 minutes for acclimatization of body temperature
- The image acquisition was performed
(Images, from each patient, were acquired in four different poses:
- front with arms raised
- front with arms down
- left side (left breast only)
- right side (right breast only)
For the analyzes performed in this work, only the frontal images with the raised arms were considered since the images in the other positions were not standardized.
The patients were classified into three groups
- Normal (without changes)
- Benign changes (benign nodules)
- Malignant changes (tumors)
The patients were only submitted to the necessary examinations so that the specialist doctor had the conclusive and final diagnosis.
Experiment
Two classifiers were considered:
- Artificial Neural Networks (ANN)
- Support Vector Machine (SVM)
Experiments were performed with three different input images. For the first one no spatial filter was applied in the images. In the second the median filter was applied while in the third a Gaussian filter with σ=2 was applied. Based on the features presented in Section 2, seven different feature combination were tested. The choice of these combinations was made based on what was presented in [3,7,8]. Feature combination are going to be presented in details in the extended version of the paper: Gonçalves, C.B; Leles, A.C.Q.; Oliveira, L.E.; Guimaraes, G.; Cunha, J.R.; Fernandes, H. Machine Learning and Infrared Thermography for Breast Cancer Detection. Proceedings 2019, 27, 45.
Results
The best result obtained with the ANN was achieved with 15 neurons in the hidden layer, considering the feature combination number. This setup had an accuracy of 76.19%, a normal specificity of 57.1%, a benign specificity of 83.3%, and a malignant sensitivity of87.5%.
For the SVM, the best result was also achieved by using the feature combination number 5. This setup had an accuracy of 80.95%, a normal specificity of 83.33%, a benign specificity of 85.71%, and a malignant sensitivity of 75%.
Conclusions
The use of infrared images for the detection of breast cancer is a promising screening technique which can aid in the diagnostic of the disease since it is a pain-free technique, can identify changes in dense breasts (which is hard for the conventional mammography), there is no harmful radiation, can identify early changes, and has a low cost.
Our results are promising and confirm that infrared images can be used for breast cancer detection. Gonçalves, C.B; Leles, A.C.Q.; Oliveira, L.E.; Guimaraes, G.; Cunha, J.R.; Fernandes, H. Machine Learning and Infrared Thermography for Breast Cancer Detection. Proceedings 2019, 27, 45.
AI Talos is an AI-powered software reinventing how thermographers all around the world can detect breast cancer using deep learning and thermal imaging methods, for more information please visit our website at www.aitalos.com or have a look at our LinkedIn public page at: https://www.linkedin.com/company/ai-talos